
A team of researchers affiliated with a large number of institutions in China has used a machine-learning algorithm with cancer methylation signatures to diagnose colorectal cancer. In their paper published in the journal Science Translational Medicine, the group describes their new approach to diagnosis and prognostication of colorectal cancer and how well it worked.
Currently, the gold standard for detecting colorectal cancer is through the use of colonoscopies—such procedures are, unfortunately, invasive, uncomfortable and embarrassing for patients. Because of that, many people forgo testing, and sadly, some develop colorectal cancer that goes undetected for long periods of time. Refusing testing is problematic because colorectal cancer is the third-most deadly kind of cancer worldwide. Scientists recognize the problem and continue to look for other ways to detect the disease. One promising area of research involves looking for markers of the disease in blood, which would be far less invasive. Unfortunately, such tests are still not as effective as colonoscopies. In this new effort, the researchers looked at the possibility of combining two diagnostic tools to improve accuracy.
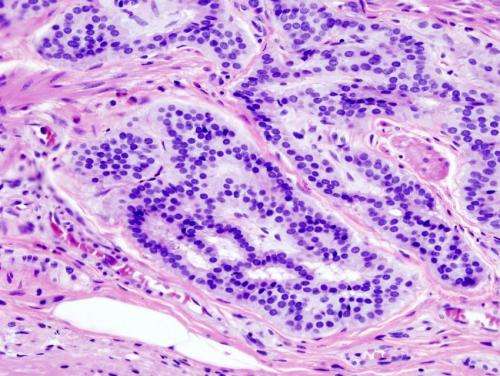
The first diagnostic tool involved identifying colorectal cancer-specific methylation signatures. The researchers did this by comparing cancer tissue from people with colorectal cancer and from those without—more specifically, they looked for circulating tumor DNA (ctDNA) differences. Once they had their markers, the team used a machine-learning algorithm to spot cancer in people who were at risk for developing colorectal cancer. The algorithm was trained on cell data from 801 people who had colorectal cancer and from 1,021 people who did not, and learned to distinguish between cell types. Once the system had learned what to look for, the researchers tested it on patients known to have colorectal cancer. The researchers report that the system was 87.5 percent and 89.9 percent accurate when testing for sensitivity and specificity.
Source: Read Full Article