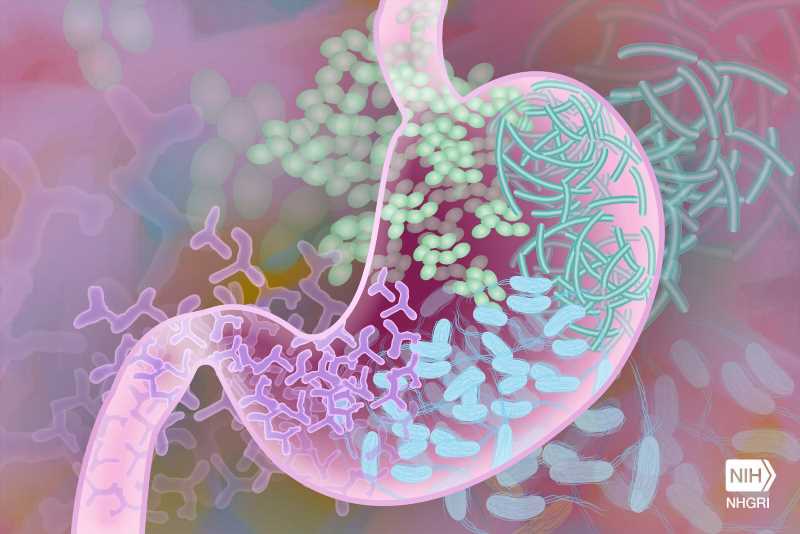
Recurrent bouts of systemic lupus erythematosus, marked by the body’s immune system attack of its own tissues, closely tracked with measureable upticks in growth in the gut of a certain species of bacteria.
New research from NYU Grossman School of Medicine shows that bacterial blooms of the gut bacterium Ruminococcus blautia gnavus occurred at the same time as disease flare-ups in five of 16 women with lupus of diverse racial backgrounds studied over a four-year period. Systemic lupus erythematosus involves damaging inflammation, especially in the kidneys, but also in joints, skin, and blood vessels. Four of these study patients with R. gnavus blooms had severe cases of the most common and kidney-specific form of the disease, lupus nephritis, while one had a severe example of lupus involving inflammation in multiple joints.
Publishing in the Annals of Rheumatic Diseases online June 27, the team’s analysis of these lupus patients’ gut bacterial blooms identified 34 genes that already had established links to the bacterium’s growth in people with inflammation. While the specific causes of lupus, which affects as many as 1.5 million Americans, remain unknown, many experts suspect that bacterial imbalances trigger inherited genetic factors responsible for the disease.
This study also investigated how tightly these patients’ immune system antibodies bonded to structures in the bacterial wall, much like they would an invading virus. These antibodies showed a strong affinity to specific bacterial lipoglycan molecules that are known triggers of inflammation. These lipoglycans were found to be common in R. gnavus strains in lupus patients but not in healthy people. Antibodies are a major cause of the body damage in this disease, and this diagnostic antibody response, the researchers say, highlights the important role played by R. gnavus in the autoimmune disease.
“Our findings provide the strongest evidence to date that silent growths of Ruminococcus blautia gnavus are tied to active serious renal disease in lupus patients,” said study lead investigator Doua Azzouz, Ph.D.
“Interestingly, our study also established this common bacterial link among a racially diverse group of females with varying forms of lupus,” said Azzouz, a postdoctoral researcher in the Department of Medicine at NYU Langone Health. Lupus is more common in women than in men, and the disease affects more Blacks, Hispanics, and Asians than Whites.
“Our goal is to use our growing understanding of the biological pathways that underpin the disease to develop new treatments that prevent or treat flares for all forms of lupus,” said study senior investigator and immunologist Gregg Silverman, MD.
“Such future treatments for lupus, especially lupus nephritis, could potentially decrease the use of drugs designed to dampen the immune system and instead promote the use of less-toxic antibacterial agents, probiotics or dietary regimens that prevent imbalances such as Ruminococcal blooms in the local gut bacterial population, or microbiome,” said Silverman, the Mamdouha S. Bobst Professor of Internal Medicine in the Departments of Medicine and Pathology at NYU Langone Health.
Previous research by Silverman’s team showed that R. gnavus blooms weaken the gut wall barrier, prompting bacterial leakages that in turn trigger inflammatory and overactive immune responses.
Silverman, who also serves as associate director of rheumatology at NYU Langone, says the team plans to extend the current research to more patients at other medical centers. The team also has plans for further experiments in mouse models of lupus to see how R. gnavus colonization triggers lupus and whether in mice bred to develop lupus-like symptoms R. gnavus blooms speed up or otherwise affect the severity of flares and inflammation.
The researchers say they also want to conduct experiments on various lipoglycan molecules from different R. gnavus strains to see if any particular part of the molecular structure is key to triggering inflammation or if other lipoglycans also prompt an immune response tied to lupus or other diseases of the gut, including Crohn’s.
For the study, researchers used stool and blood samples from lupus patients being treated at NYU Langone. All study participants were being closely monitored for disease flare-ups. Test results were compared with those of 22 female volunteers of similar age and racial background who did not have lupus and were otherwise healthy.
As an autoimmune disease, systemic lupus erythematosus can lead to widespread inflammation and long-term tissue damage in affected organs. According to researchers, about half of patients develop lupus nephritis, of whom one-quarter are likely to experience end-stage renal disease that may require regular blood dialysis and even kidney transplantation.
Besides Silverman, other NYU Langone researchers involved in this study are Ze Chen, Peter Izmirly, Lea Ann Chen, Zhi Li, Chongda Zhang, Adriana Heguy, Davis Mieles, Kate Trujillo, Alejandro Pironti, Gregory Putzel, David Fenyo, and Jill Buyon. Other study co-investigators are Dominik Schwudke and Nicolas Gisch, at the Leibniz Lung Center in Borstel, Germany; and Alexander Alekseyenko at the Medical University of South Carolina in Charleston.
More information:
Doua Azzouz et al, Longitudinal gut microbiome analyses and blooms of pathogenic strains during lupus disease flares, Annals of the Rheumatic Diseases (2023). DOI: 10.1136/ard-2023-223929
Journal information:
Annals of the Rheumatic Diseases
,
Annals of Rheumatic Diseases
Source: Read Full Article