
A research team at LKS Faculty of Medicine, The University of Hong Kong (HKUMed) reports that exosomes derived from Vδ2-T cells (Vδ2-T-Exos) can effectively control Epstein-Barr-virus-associated tumors and induce T-cell anti-tumor immunity. The novel findings of Vδ2-T-Exos provide insights into a new therapeutic approach for Epstein-Barr virus (EBV)-associated tumors. The groundbreaking findings have been published in the leading academic journal Science Translational Medicine.
EBV infects about 95% of the human population and causes more than 200,000 cases of cancer each year, and that around 2% of all cancer deaths are due to EBV-attributable malignancies. EBV-associated tumors include Burkitt lymphoma, Hodgkin’s lymphoma, nasopharyngeal carcinoma, gastric tumors and post-transplant lymphoproliferative disease, etc.
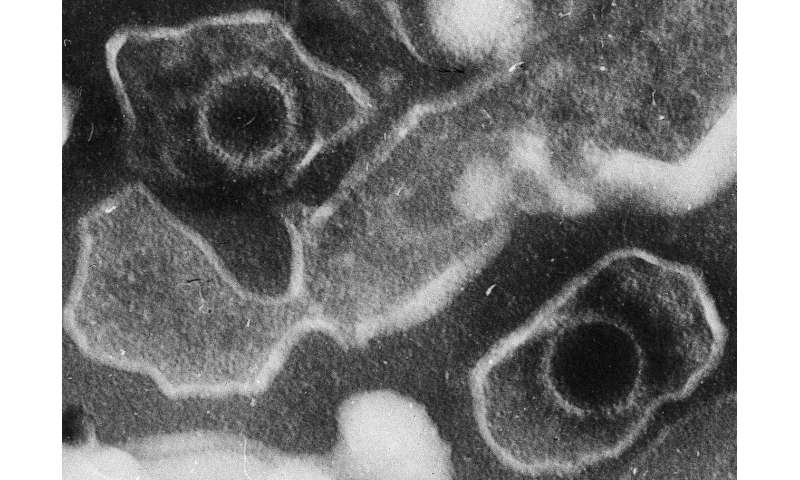
Current treatment options for EBV-associated tumors are limited with considerably unwanted off-target toxicities and incomplete effectiveness for relapsed or refractory disease. Vδ2-T cells are innate-like T cells with anti-tumor potentials against EBV-associated tumors. Unfortunately, its clinical translation is limited because Vδ2-T cells from some cancer patients are difficult to expand. Exosomes are endosome-originated small extracellular vesicles that mediate intercellular communication. Compared with cell-based therapy, cell-free exosomes have advantages with higher safety, easier storage, and lower costs. However, the anti-tumor activity of exosomes derived from Vδ2-T cells (Vδ2-T-Exos) remains unknown.
The team found that Vδ2-T-Exos contained death-inducing ligands (FasL and TRAIL) and immunostimulatory molecules (CD80, CD86, MHC class I and II). Vδ2-T-Exos targeted and efficiently killed EBV-associated tumor cells through FasL and TRAIL pathways and promoted EBV antigen-specific CD4 and CD8 T cell expansion. Administration of Vδ2-T-Exos effectively controlled EBV-associated tumors in immunodeficient and humanized mice.
Because expanding Vδ2-T cells and preparing autologous Vδ2-T-Exos from cancer patients ex vivo at a large scale is challenging, the team further explored the anti-tumor activity of allogeneic Vδ2-T-Exos in humanized mouse cancer models. Interestingly, the team found that allogeneic Vδ2-T-Exos had more effective anti-tumor activity than autologous Vδ2-T-Exos in humanized mice; the allogeneic Vδ2-T-Exos increased the infiltration of T cells into tumor tissues and induced more robust CD4 and CD8 T cells-mediated anti-tumor immunity. Compared with exosomes derived from NK cells with direct cytotoxic anti-tumor activity or dendritic cells that induced T-cell anti-tumor responses, Vδ2-T-Exos have dual anti-tumor activities by directly killing tumor cells and indirectly inducing T cell-mediated anti-tumor responses, thus resulting in more effective control of EBV-associated tumors.
“Our study provides the first evidence about the anti-tumor activities of Vδ2-T-Exos against EBV-associated tumors. These exosomes could effectively control EBV-associated cancers in multiple mouse models. More importantly, allogeneic Vδ2-T-Exos had higher therapeutic efficacy than autologous Vδ2-T-Exos to control EBV-associated tumors. Therefore, the Vδ2-T-Exos prepared from healthy donors can be used to treat patients with EBV-associated tumors, which is highly beneficial to the clinical application of this novel approach,” said Professor Tu Wen-wei, Antony and Nina Chan professor in Pediatric Immunology, Department of Pediatrics and Adolescent Medicine, HKUMed, who led the research.
Source: Read Full Article