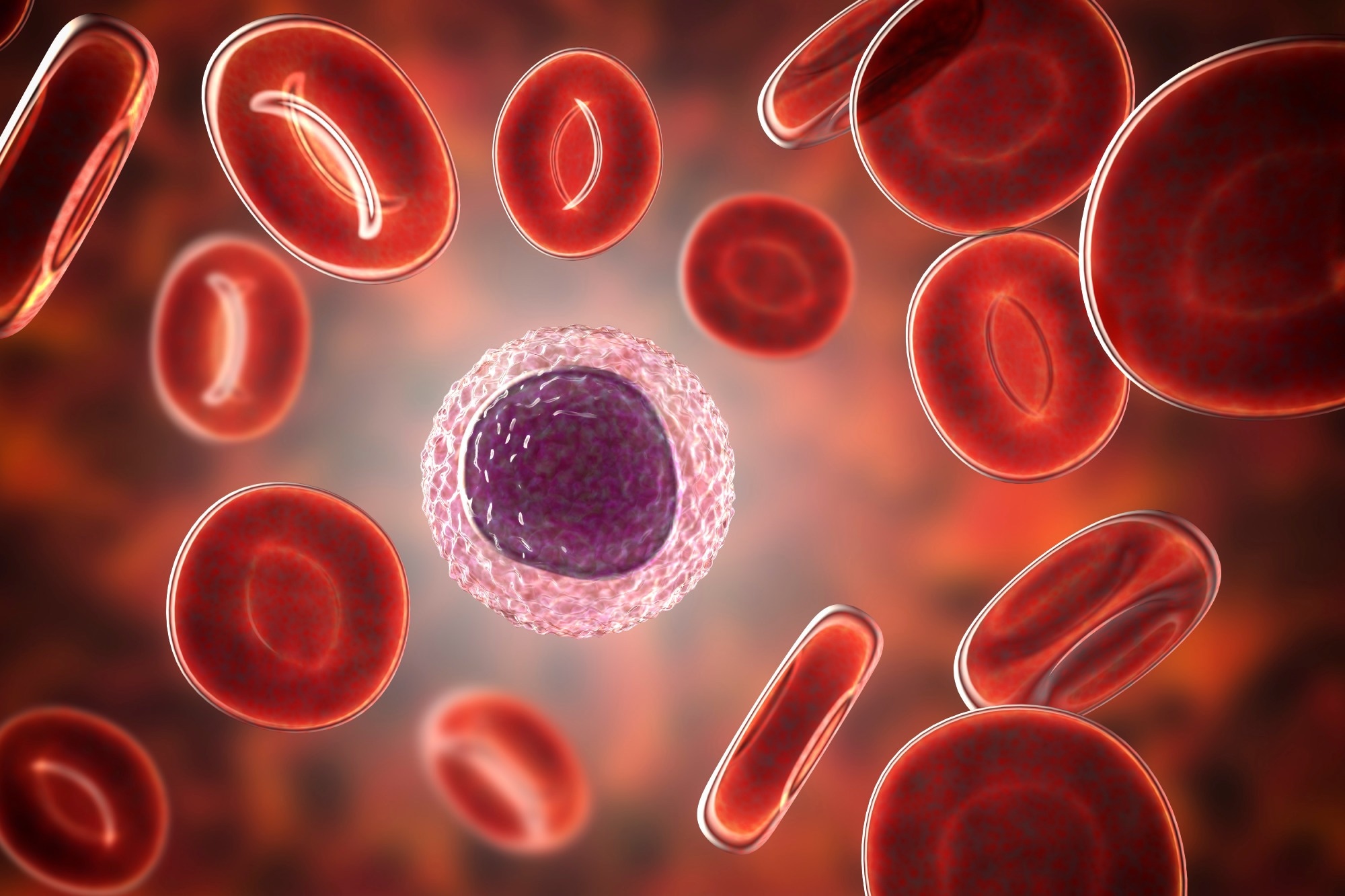
Agammaglobulinemia is a set of inherited immunological disorders marked by low antibody levels in the blood due to a lack of certain lymphocytes in the blood and lymph.
While X-linked agammaglobulinemia (XLA) is the most frequent cause of congenital agammaglobulinemia, accounting for about 85% of cases, other genetic types of agammaglobulinemia have been discovered.
X-linked agammaglobulinemia (XLA), autosomal recessive agammaglobulinemia (ARAG), and autosomal dominant agammaglobulinemia are the three kinds of agammaglobulinemia.
Serial bacterial infections are the main symptoms of agammaglobulinemia, which are caused by deficiencies in certain immunological responses caused by abnormalities in B-lymphocytes. Infections commonly occur in the gastrointestinal tract, lungs, skin, joints, and upper respiratory tracts.
XLA
A mutation in Bruton's tyrosine kinase (BTK) causes this X-linked agammaglobulinemia. BTK is a cytoplasmic tyrosine kinase that is mostly expressed in hematopoietic cells. There have been over 600 mutations discovered in BTK, with the bulk of them involving 1–4 base pairs.
Recurrent, pyogenic bacterial infections in young boys and a near-complete absence of all immunoglobulin isotypes are among the clinical manifestations of XLA. Streptococcus pneumoniae, Staphylococcus spp., Pseudomonas spp., and Haemophilus influenzae are among the most prevalent pathogens found in XLA.
Prior to diagnosis, recurrent otitis is the most frequent infection. In addition, conjunctivitis, sinopulmonary infections, diarrhea, and skin infections are common.
When people with XLA acquire a serious, life-threatening condition such as pneumonia, empyema, meningitis, sepsis, or septic arthritis, they are diagnosed with immunodeficiency. Neutropenia has been identified as a prevalent XLA symptom.
The prevalence of XLA varies between 1:100,000 and 1:200,000. There is no known ethnic predilection, but the White race has the highest documented occurrence. Males with early-onset bacterial infections, substantial reductions in all classes of blood immunoglobulins, and missing B cells are suspected of having XLA.
The prognosis for people with XLA has improved dramatically in the last 25 years as a result of earlier diagnosis, the discovery of gammaglobulin preparations that allow for normal blood IgG concentrations, and more liberal antibiotic use.
Autosomal recessive and autosomal dominant agammaglobulinemia
In comparison to XLA, autosomal recessive agammaglobulinemia is a rare cause of agammaglobulinemia. Mutations have been found in the mu heavy chain, Lambda 5, Ig alpha, Ig beta, BLNK, PI3K, and TCF3 genes so far. Due to mu heavy chain mutations, BLNK insufficiency, and Ig alpha deficit, neutropenia has been found in some ARA patients. These diseases are more severe and manifest earlier than XLA instances. Some patients with early B cell developmental abnormalities have yet to be diagnosed with a genetic etiology, though this is changing because of breakthroughs in diagnostic and genetic testing.
Mutations in numerous different genes have been linked to autosomal recessive agammaglobulinemia, including the heavy chain gene, 5, Ig, Ig, BLNK, PIK3R, and TCF3. Mutations in the LRRC8A gene on chromosome 9q34 and the TCF3 gene on 19p13.3 have been linked to autosomal dominant agammaglobulinemia.
Diagnosis and treatment
Immunoglobulin levels are measured in blood tests to confirm the condition. Flow cytometry, immunoelectrophoresis, and nephelometry to quantify immunoglobulins (IgG, IgA, IgM) are among the tests used to determine the number of circulating B lymphocytes.
The presence of a missing B cell in a maternal uncle or male cousin essentially guarantees the diagnosis. Males with a hemizygous BTK pathogenic mutation and females with a heterozygous BTK pathogenic variant have their XLA diagnosis confirmed.
Treatment entails taking actions to limit the number of infections and their severity. Bacterial infections frequently necessitate the use of antibiotics. Immunoglobulins are injected or given through a vein to enhance the immune system. A bone marrow transplant is a possibility.
Molecular genetic testing of at-risk male relatives as soon as feasible after delivery guarantees that affected individuals receive gammaglobulin substitution therapy as soon as possible.
Corticosteroids and other immune-suppressing medicines (immunosuppressant drugs) should be avoided as much as possible. Patients should also avoid strenuous activity that could harm their spleen, such as harsh contact sports.
Immunoglobulin replacement comes in a variety of forms and can be given intravenously or subcutaneously. The patient receives intravenous immunoglobulin replenishment every 3–4 weeks. Although no current published guidelines exist, prophylactic antibiotics can be used to avoid infection.
Prophylactic antibiotics may be considered, especially if patients continue to get infections despite receiving appropriate immunoglobulin replacement therapy.
Agammaglobulinemia in COVID-19 patients
With the outbreak of the SARS-CoV-2 pandemic in 2019, it is expected that immunocompromised patients will be particularly vulnerable. Patients with agammaglobulinemia with coronavirus disease 2019 (COVID-19) infection have been described in a small number of cases.
Seven patients, one with XLA, one with autosomal recessive agammaglobulinemia, and five with CVID (common variable immune deficiency) with COVID, were described by a group of researchers. The investigators reported that the two patients with agammaglobulinemia had mild clinical outcomes, but the five with CVID had severe disease and one fatality.
Another study identified two patients with XLA who developed COVID-19 with a complete lack of B lymphocytes in their peripheral blood. According to their findings, XLA patients are at a higher risk of developing pneumonia as a result of SARS-CoV-2 infection, but they can recover.
While additional research is needed, observations and case reports have revealed that certain people with XLA had a milder type of COVID-19 than those with other underlying immunodeficiencies.
References
- Cardenas-Morales M, & Hernandez-Trujillo, VP (2021). Agammaglobulinemia: from X-linked to Autosomal Forms of Disease. Clinical Reviews in Allergy & Immunology, 1–14. Advance online publication. doi: https://doi.org/10.1007/s12016-021-08870-5
- Lackey AE, Ahmad F. X-linked Agammaglobulinemia. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549865/
- Soresina A, Moratto D, Chiarini M, et al. (2020). Two X-linked agammaglobulinemia patients develop pneumonia as COVID-19 manifestation but recover. Pediatric Allergy and Immunology: Official Publication of the European Society of Pediatric Allergy and Immunology, 31(5), 565–569. doi: https://doi.org/10.1111/pai.13263
- El-Sayed ZA, Abramova I, Aldave JC, et al. (2019). X-linked agammaglobulinemia (XLA): Phenotype, diagnosis, and therapeutic challenges around the world. The World Allergy Organization Journal, 12(3), 100018. doi: https://doi.org/10.1016/j.waojou.2019.100018
- Suri D, Rawat A, & Singh S (2016). X-linked Agammaglobulinemia. Indian Journal of Pediatrics, 83(4), 331–337. doi: https://doi.org/10.1007/s12098-015-2024-8
- Smith C, & Berglöf A (2001). X-Linked Agammaglobulinemia. In M. P. Adam (Eds.) et. al., GeneReviews®. University of Washington, Seattle. https://europepmc.org/article/NBK/nbk1453
- Agammaglobulinemia. [Online] Medline Plus. Available at: https://medlineplus.gov/ency/article/001307.htm#:~:text=Agammaglobulinemia%20is%20an%20inherited%20disorder,more%20likely%20to%20get%20infections.
Further Reading
- All Immunology Content
- What is Immunology?
- What does it mean to be Immunocompromised?
- Classical Immunology
- The Immunological Functions of Red Blood Cells
Last Updated: Sep 5, 2023