
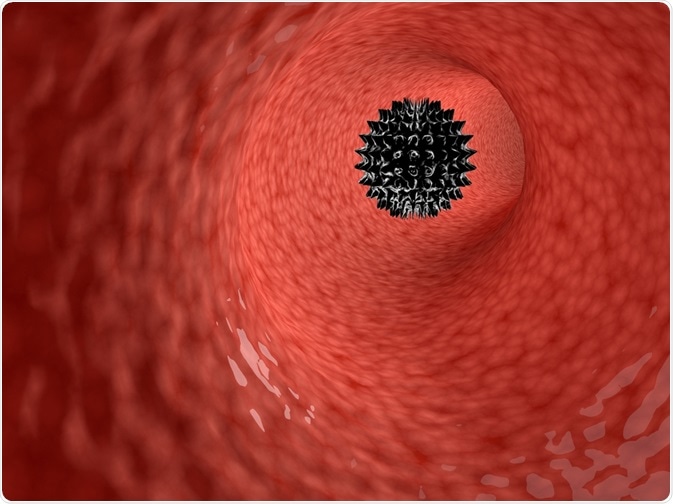
Sepsis is a globally occurring disease state that can occur when the body is infected with bacteria, virus, fungi or parasites.
Sepsis occurs when the body's immune system reacts systemically to an infection, causing injury to tissue and organs. It is a highly serious condition with the potential to be fatal.
There is no singular pathophysiology to sepsis, as sepsis can be manifested by several symptoms and through several pathways.
Basic Pathophysiology
Sepsis starts with an infection of a microorganism, such as a bacteria or virus. In bacterial infections, Gram-positive bacteria have been shown to be more common than Gram-negative bacterial infections.
Different types of bacteria or pathogen have different effects on the body and may therefore alter the pathophysiology of sepsis slightly.
Endotoxins on Gram-positive and Gram-negative bacteria trigger a reaction from the immune system.
Macrophages are a particular target and it is the targeting of macrophages which leads to production of mediators of inflammation. One of the most commonly implicated mediators in sepsis is tumor necrosis factor alpha (TNF-α).
Exotoxins released from Gram-positive bacteria target T-lymphocytes instead of macrophages. This results in the T-lymphocytes producing interleukin 2 (IL-2) and interferon gamma (IFN-γ). These together trigger macrophages to release IL-1 and TFN-α, which are critical for creating an inflammatory response.
The mediators that are produced help facilitate an inflammatory reaction or an anti-inflammatory one.
There is evidence to suggest that while the start of sepsis seems to implicate mediators causing an inflammatory reaction, it changes to an anti-inflammatory suppressed immune system state as sepsis endures.
However, the type of mediator secreted and thus the type of reaction, overwhelmingly inflammatory or anti-inflammatory, can depend on the type of pathogen and the location of infection.
Circulation
Blood circulation through the body is normally controlled by homeostatic mechanisms keeping the blood in a liquid state and allowing it to flow through blood vessels.
During sepsis there is often disseminated intravascular clotting (DIC), meaning platelets are clotting the blood inside the vessels. This also means platelets and clotting factors are used up, which can lead to extended bleeding if an injury occurs.
The underlying cause of the malfunctioning coagulation, also called coagulopathy, is not fully known. The coagulation can depend on the endothelium, the clotting system, and the platelets.
Certain pro-inflammatory mediators can stimulate clotting by increasing coagulation factors in tissues and membrane coagulants, as well as by inhibiting anticoagulant activity. Anti-inflammatory mediators, on the other hand, inhibit activation of the clotting system.
Immune Responses
The inflammatory response plays a central role in sepsis. It was long believed that microorganism infection triggered an immune response, as it should, but the body responds either excessively or fails to respond to the infection.
It was initially believed this was due to increased production of proinflammatory molecules, due to the implications of mediators such as TNF in septic patients and the sepsis-like effects seen when TNF was injected into experimental animals.
While many treatments, particularly TNF-inhibition focused ones, have been tried with little success in terms of survival rates; exploration of other mediators is encouraged as several mediators with strong potential remain unexplored.
It is also highlighted that cytokines, a group of immune-related substances including growth factors, can have effects on the local level without being detectable at plasma level and may therefore have evaded our radar.
Another central theory to sepsis is the opposite of excessive proinflammatory molecules – suppression of an appropriate immune response. Immune response mediators such as TNF have been shown to be reduced in some patients with sepsis, whereas anti-inflammatories such as interleukin 10 (IL-10) have not been affected.
There is then an imbalance between proinflammatory and anti-inflammatory responses, leading to a net effect where the inflammatory response is diminished.
Treatments focusing on stimulating the immune response have had mixed success, just like the immunosuppressants. Stimulating treatments have not improved survival rate but have shortened time spent in hospital.
The results therefore seem to be complex as to the immune-related pathophysiology sepsis has. Some patients seem to benefit from immunosuppressants, while others require immunostimulants. Whereas other diseases benefit from treatment that is tailored, this approach has not been widely used in sepsis.
The long-favored theory that sepsis is an uncontrolled inflammatory response to a pathogen may still hold merit, while alternative theories showing the diverse nature of sepsis are gaining traction.
Sources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1854939/
- https://www.ncbi.nlm.nih.gov/pubmed/12519925
- https://www.ncbi.nlm.nih.gov/pubmed/24295606
Further Reading
- All Sepsis Content
- Everything You Need To Know About Sepsis
- Sepsis Diagnosis
- Causes and Symptoms of Sepsis in Newborns
- Diagnosis and Treatment of Sepsis in Newborns
Last Updated: Sep 10, 2018

Written by
Sara Ryding
Sara is a passionate life sciences writer who specializes in zoology and ornithology. She is currently completing a Ph.D. at Deakin University in Australia which focuses on how the beaks of birds change with global warming.
Source: Read Full Article