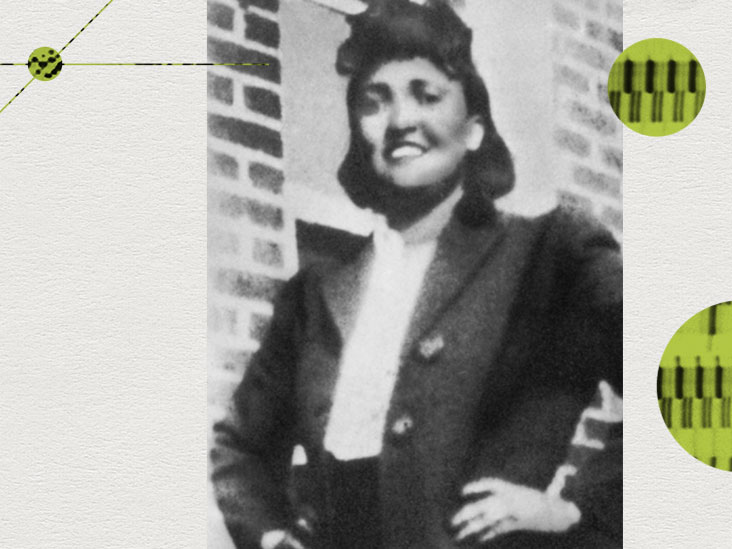
In the past century, Henrietta Lacks has, arguably, done more to advance medicine than any other person. She played a material role in the development of polio vaccines, cancer treatments, HPV vaccines, and mapping the human genome. This young Black woman died from cervical cancer in 1951. It was cells taken during her cancer treatment that became one of the most powerful research tools ever, but she did not know about or give permission for their retrieval. What can we learn from such wrongs committed in the name of science?

In January 1951, a few months after giving birth to her fifth child, Henrietta Lacks, a 30-year-old Black woman, became concerned about a lump on her cervix. This, and unexplained vaginal bleeding, led her to seek medical attention.
She went to Johns Hopkins in Baltimore, the only hospital in the area that would provide treatment to Black people at that time.
Doctors there diagnosed a particularly aggressive form of cervical cancer. She did not tell her husband or family, informing them only that she had to go to the doctor for medicine.
The standard treatment at the time was radium therapy. During her first treatment, under sedation, the surgeon took a tissue sample from her tumor. He passed this on to the head of tissue culture research at Johns Hopkins, Dr. George Otto Gey.
“When Henrietta Lacks sought care at Johns Hopkins University — one of the few segregated hospitals to serve Black patients in Baltimore, MD, at the time — a biopsy of her cervical cells was extracted to diagnose her cervical cancer. The original doctor did not keep her sample for his own research but immediately shared it broadly with the larger scientific community. In 1951, the informed consent process as we now know it did not exist to protect patient privacy, rights or govern scientific and clinical research.”
– Dr. Maranda C. Ward, assistant professor and director of Equity, Department of Clinical Research and Leadership, School of Medicine and Health Sciences, The George Washington University
Taking cell samples for research was routine practice at the time, and doctors rarely asked patients for consent. As a result, most patients were, like Henrietta, completely unaware of what would happen to their cells.
An uneasy immortality
The cells that doctors took from Henrietta’s tumor were then placed in a culture medium, labeled “HeLa” to identify them. The researchers expected that, like most cell samples, they would multiply a few times, then die.
After her first treatment, doctors discharged Henrietta from the hospital, and she went back to work in the tobacco fields, oblivious to the fact that doctors had taken her cells for research purposes.
In the lab, the HeLa cells not only remained alive, but multiplied at an astonishing rate.
Dr. Gey informed colleagues that his lab had grown the first immortal cell line, and shared samples of HeLa cells with them.
“What was done to her, the reuse of her information, the attaching of her name to the cells — the HeLa cells are named after her — that’s a massive violation of her privacy. All of those practices are of a bygone era where consent and privacy were just not taken as seriously or even thought about at all.”
– Dr. Sean Valles, director and associate professor, Center for Bioethics and Social Justice, Michigan State University
Although Henrietta’s initial treatment led to the tumor shrinking, by September, her cancer had spread to many of her internal organs.
Henrietta Lacks died, aged just 31, on October 4, 1951, unaware that she had unwittingly left behind an extraordinary legacy.
The power of HeLa cells
Some 70 years on, the cell line from the original HeLa cells is still proliferating. In that time, more than 11,000 research publications have involved HeLa cells.
In 1953, two researchers from Tuskegee University cultured HeLa cells, and mass-produced them for use throughout the United States in the development of the first successful polio vaccine.
Later in the 1950s, researchers used the cells to investigate the effects of X-rays, and to develop a method, still used today, of testing whether cells are cancerous.
Cells from the HeLa line have also been sent into space, used to investigate the effects of space travel and radiation on human cells, used to determine how Salmonella causes infections, to investigate blood disorders, to advance understanding of HIV, and in unraveling the secrets of the human genome.
Only some of the research stated that HeLa cells had been used.
Most pertinently, given that Henrietta Lacks died from cervical cancer, HeLa cells were vital in discovering how HPV causes cervical cancer, and in the development of the vaccine against HPV.
It is particularly troubling that, as Dr. Valles stated: “In the U.S., Black women have especially poor outcomes with cervical cancer, because that’s why she went to the hospital in the first place. They’re seeing the doctor, but they’re not getting treated in a timely way.”
Dr. Harald zur Hausen, an author on the HPV study, went on to win the 2008 Nobel prize in Physiology or Medicine for his work on viruses and cancer.
This was just the first of three Nobel prizes from research using HeLa cells, the others being for research on telomeres in 2009, and live viewing of cellular growth in 2014.
What made HeLa cells unique?
Unlike almost all other cell samples, HeLa cells continued to replicate in cell culture and the line has survived for more than 70 years. So what was it about these cancer cells that made them so powerful?
Although scientists do not fully understand what gives HeLa cells their unique properties, research has shown that there are three ways in which HeLa cells are different from normal human cells:
- HeLa cells have 76 to 80 chromosomes, whereas normal human cells have 46. This is a result of infection with HPV which causes errors in the genome to accumulate as uncontrolled division occurs.
- HeLa cells grow even faster than most cancer cells, so if they contaminate other cell cultures they overtake them. Researchers attribute this to the fact that Henrietta Lacks also had syphilis, which weakens the immune system and allows cancers to grow aggressively.
- HeLa cells can divide an infinite number of times as their telomeres regrow after each division. In normal cells, telomeres decrease at each division, leading to cells aging and dying.
Whatever the reason, HeLa cells have proved a vital tool in biomedical research.
Inequality and a historic wrong
“Henrietta also experienced the untreated effects of syphilis on the birth outcomes of her children before seeking out care for unexplained abdominal pain, which doctors described as impacting her disease prognosis once they identified her cancer. So, racism, gender oppression, and poverty most certainly shaped her life chances and opportunities for health.”
– Dr. Maranda Ward
Henrietta Lacks’ cells played a material role in work that led to three Nobel prizes and many other scientific discoveries — but they were used and shared without consent from her, or from any member of her family.
At the time, permission was neither required, nor sought, for cells to be used for research.
This was normal procedure in the 1950s, as Dr. Valles pointed out: “There was non-consensual research happening everywhere, because consent didn’t really matter, but it always happens to be the case that people being burdened by this, people being taken advantage of, disproportionately end up being Black Americans […] something happens, and it works out worse for this population.”
“The billion-dollar industry tied to the immortal HeLa cell line is yet another example of how the U.S. has exploited and profited off the bodies of Black people. Once informed consent processes established that obtaining and researching the HeLa cells was unethical because it violated human rights, privacy, and bodily autonomy, its continued use represented a blatant disregard for Henrietta’s humanity, let alone scientific integrity and ethical conduct of research.”
– Dr. Maranda Ward
How the case came to light
For around 25 years, researchers used HeLa cells without any acknowledgment of where they had originated.
Then, in 1976, a reporter, Michael Rogers, uncovered the origin of the name HeLa, revealing in Rolling Stone magazine that the cells were from Henrietta Lacks.
And it was only then, long after her cells had been shared around the world and played a part in many medical breakthroughs, that her family became aware of what had happened.
Some years later, Rebecca Skloot, an investigative journalist, picked up the story. She contacted Henrietta’s family, who were at first reluctant to talk to her. Eventually, she persuaded Henrietta’s youngest daughter, Deborah, to provide personal insight into her mother’s story.
Skloot’s book, The Immortal Life of Henrietta Lacks, was published in 2010, and made into a film in 2017.
Following the publication of her book, Rebecca Skloot established the Henrietta Lacks Foundation, with the purpose of “[h]elping individuals who have made important contributions to scientific research without personally benefiting from those contributions, particularly those used in research without their knowledge or consent.”
Several of Henrietta Lacks’ descendants have been helped by the foundation — one small step, perhaps, in making reparation for the wrong done to Henrietta Lacks.
Is consent enough?
In the U.S., the Common Rule, instigated in 1981 and updated since, sets out ethical guidelines for biomedical and behavioral research involving humans. Among other issues, it covers compliance, record keeping, and, most importantly, informed consent.
A 2013 paper described the role of informed consent in research as the “[b]asic ethical principle behind informed consent legalities is to protect the autonomy of human subjects which states that welfare and interests of a subject participating into clinical research are always above the society’s interests and welfare. Medical research directed towards treatment advances for society’s benefit and betterment can never be built on sacrificing the rights and health of research participants.”
However, as Dr. Ward noted, the consent system is imperfect:
“Current consent procedures are highly varied and therefore remain inadequate. This partly explains why the U.S. health goals (Healthy People 2030) include a new aim to attain health literacy. We recognize that we will not be able to eliminate health disparities and achieve health equity if patient populations do not know where to access credible health information or make sense of the information they do receive for what it means for their own health.”
“I do believe not enough attention is paid to the right to refusal as a part of informed consent nor is the idea that you can change your mind and withdraw participation at any point without any effect to the relationship with the clinical team or type of care you receive,” she added.
Henrietta Lacks, like so many others, had no right to refusal.
A lack of trust
“Henrietta Lacks was taken advantage of and the fruits of her body were taken without her knowledge and without her consent, and even after all these decades of improvements of the American medical system and the system worldwide, somehow still, people who are black Americans, like Henrietta Lacks, are still disadvantaged.”
– Dr. Sean Valles
This is just one case that has damaged trust in medical science among Black, American Indian, and people of color, in general, in the U.S.
It came in the midst of the Tuskegee Syphilis study where between 1932 and 1972 doctors denied treatment to Black men with syphilis — even after penicillin was identified as an effective cure — so that they could study the course of the disease.
More recently, during the COVID-19 pandemic, in both the U.S. and the United Kingdom people of color were at far greater risk of mortality than white people. In the U.K., Black African men were 3.7 times more likely to die from COVID-19 than white men.
And according to the CDC, Black or African American, American Indian or Alaska Native, and Hispanic or Latino individuals were around twice as likely to die from COVID-19 than white people.
Has there been an effort to earn back that lost trust? Dr. Valles is not convinced, asking: “What has the biomedical system, whether it’s individual hospitals, like Johns Hopkins University Hospital, or any other university hospital, what have they done to earn the trust of people who don’t trust them?”
The way ahead
Currently, most research is carried out in white, educated, industrialized, rich, democratic (WEIRD) people. Scientists have acknowledged that such data are not representative, and that research must include data from diverse populations.
“These are the privileged social identities that default as the standard of health within Westernized medicine and codified as metrics for what gets valued. Until scientists and researchers center the experiences of Black women — the most disrespected and categorically disadvantaged U.S. group — racial injustice — and therefore — uneven and unfair opportunities for health will persist.”
– Dr. Maranda Ward
Henrietta Lacks was taken advantage of because, perhaps, doctors thought she did not matter. Her cells were just tools for research. We might hope that such attitudes are a thing of the past, but inequity still exists.
Dr. Ward commented: “Medical and scientific research needs to first understand what equity is before they can apply an equity lens to their research. Equity has become a buzz term for some — resulting in it being used erroneously and interchangeably with concepts of ‘diversity’ and ‘inclusion’.”
“If a researcher understands that macro social issues such as segregation, mass incarceration, poverty, and racism are at the root of unfair health differences, their research will be designed to mitigate social and economic barriers that patients face when accessing healthcare let alone accessible and ethical research. This is what equity looks like,” she added.
Henrietta Lacks became known because of the wrong done to her in the name of science. Perhaps her most lasting legacy will be to raise awareness of the inequities in health provision and research and lead the way to a fairer, more inclusive healthcare system.
Source: Read Full Article