An investigational natural killer cell (NK) therapy has shown promise in the treatment of Alzheimer’s disease (AD), in a small phase 1 proof-of-concept clinical trial.
SNK01, being developed by NKGen Biotech, is an autologous, nongenetically modified NK cell product that has enhanced cytotoxicity and activating receptor expression.
“When we give these enhanced natural killer cells intravenously, not only do they get into the brain, but we’ve shown, through CSF biomarker data, that they reduce both amyloid and tau proteins and dramatically reducing the neuroinflammation,” Paul Song, MD, chief executive officer of NKGen Biotech, told Medscape Medical News.
“Remarkably,” in the first 6 months, 90% of patients with AD demonstrated improvement or maintained stable cognitive function, based on the AD Composite Score (ADCOMS), suggesting that SNK01 may do more than simply slow disease progression, Song said.
The findings were presented at the 16th Clinical Trials on Alzheimer’s Disease (CTAD) conference.
Sound Rationale
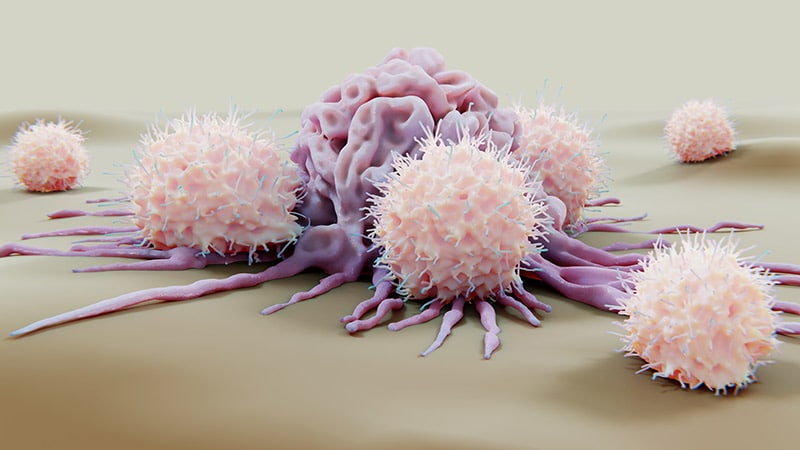
NK cells are an essential part of the innate immune system that can shape the adaptive response by eliminating activated (not resting) autologous CD4+ T cells.
Weak or deficient NK cells have been found to correlate with various diseases, including autoimmune diseases, and emerging data suggest an autoimmune component to AD.
The phase 1 study evaluated the safety, tolerability, and exploratory efficacy of SNK01 given intravenously in escalating doses every 3 weeks (four treatments in total).
Participants included 10 patients with AD confirmed by imaging. Five had mild AD, 3 had moderate AD, and 2 had advanced AD, based on baseline Clinical Dementia Rating-Sum of Boxes (CDR-SB) scores. Median baseline CDR-SB score was 9 (range, 4-18).
Cognitive Assessments included CDR-SB, Mini-Mental State Examination (MMSE), AD Assessment Scale-Cognitive Subscale (ADAS-Cog) and ADCOMS. CSF biomarker analyses were performed at baseline and at 1 and 12 weeks after the final dose (weeks 11 and 22, respectively).
NK cells were successfully activated and expanded in all 10 patients and no treatment-related adverse events were observed.
Based on the CSF biomarker data, SNK01 crossed the blood–brain barrier and reduced CSF amyloid-beta 42/40 and pTau181 levels and neuroinflammation, as measured by glial fibrillary acid protein (GFAP), and the effects appeared to persist 12 weeks after the final dose.
The exploratory efficacy data show that, one week after final dose (week 11), compared with baseline, 30% of patients showed clinical improvement on the composite ADCOMS and 60% had a stable ADCOMS score; 50% to 70% of patients were stable or improved on the CDR-SB, ADAS-Cog and/or MMSE.
“One patient went from a MMSE score of 14, which is moderate dementia, to 22, which is mild cognitive impairment,” said Song.
At 12 weeks after final dose (week 22), 44%–89% of patients remained stable or improved in all cognitive scores compared with week 11; and 50% of the patients with stable ADCOMS scores at week 11 remained stable.
Based on the positive phase 1 data, the US Food and Drug Administration (FDA) has approved a phase 1/2a study in patients with moderate AD.
“The trial will use a much higher dose and a prolonged dosing regimen and we think we’ll see even more dramatic results with more sustained higher dosing,” Song said.
Down the road, it will be interesting to see how NK cell therapy could “complement” anti-amyloid and anti-tau therapies, he added.
Ideal Treatment Approach
Commenting on this research for Medscape Medical News, Shaheen Lakhan, MD, PhD, a neurologist and researcher in Boston, said NK cells have “natural abilities that could make them an ideal treatment approach for Alzheimer’s and similar neurodegenerative diseases.”
“NK cells have properties that allow them to recognize and destroy diseased brain cells while leaving healthy cells intact, without causing excessive inflammation or autoimmune issues. It has historically been difficult to get immune cells to access the privileged immunological environment of the brain,” Lakhan explained.
“However, this line of early research shows that NK cells safely crosses the blood–brain barrier, infiltrates brain tissue, and may stave off Alzheimer’s disease as measured by biomarkers and clinical symptoms,” he noted.
“This emerging cell-based immunotherapy is highly-specific to the cells responsible for Alzheimer’s, avoids drug resistance, has long-lasting results, and has fewer side effects than drug counterparts,” Lakhan said.
The trial was sponsored by NKGen Biotech. Song and six co-authors are employees and shareholders in the company. Lakhan reports no relevant financial relationships.
16th Clinical Trials on Alzheimer’s Disease (CTAD) conference: Abstract LP129. Presented October 26, 2023.
For more Medscape Psychiatry news, join us on Facebook and Twitter
Source: Read Full Article