
Lean, metabolically unhealthy, people have a risk of cardiovascular disease (CVD) that is higher than the risk observed in obese, metabolically healthy people. Recently, novel cluster analyses (computer-based grouping of people) also identified a large heterogeneity in the risk of type 2 diabetes and CVD and of their treatment response.
These findings reveal that there may be a huge, yet undetected, treasure to be lifted in the field of cardiometabolic research. In a Review article in The Lancet Diabetes & Endocrinology, Norbert Stefan from Helmholtz Munich, the German Center for Diabetes Research (DZD) and the University of Tübingen, and Matthias B. Schulze from the German Institute of Human Nutrition Potsdam-Rehbruecke and the DZD highlight how these novel risk stratification concepts can help to better implement precision medicine in clinical practice.
Among the 20 leading global risk factors for years of life lost in 2040, the three metabolic risks—high blood pressure, high BMI, and high fasting plasma glucose—will be the top risk variables. Building upon these and other established risk factors, such as low HDL-cholesterol and high triglycides, the concept of metabolic health is attracting much attention in the scientific community. It focuses on the aggregation of important risk factors, which allows the identification of impaired metabolic health.
As of today, in most of the more than 1000 studies addressing this topic people are considered being metabolically healthy if less than 2 of the following metabolic risk factors—high blood pressure, high plasma glucose, low HDL-cholesterol and high triglycerides, or pharmacological treatment for these conditions—are present. Thereby, subphenotypes, such as people with metabolically unhealthy normal weight (MUHNW) and metabolically healthy obesity (MHO), who strongly differ in their risk of CVD, were identified.
In a meta-analysis Matthias Schulze, Norbert Stefan and colleagues found that, compared to people with metabolically healthy normal weight (MHNW), the risk of CVD is increased by 45% in people with MHO and by 100% in people with MUHNW. In their present review article Norbert Stefan and Matthias Schulze not only summarize the knowledge about these relationships, but also highlight their novel definition of metabolic health.
Considering the risk factors hypertension, diabetes and a high waist-to-hip ratio they found in two very large studies (US National Health and Nutrition Examination Survey III and UK Biobank) that the risk of CVD mortality was increased by 100% in people with MUHNW, but was not increased in people with MHO. Matthias Schulze emphasizes that “these data reveal the importance of considering the impact of body fat distribution for the definition of metabolic health.”
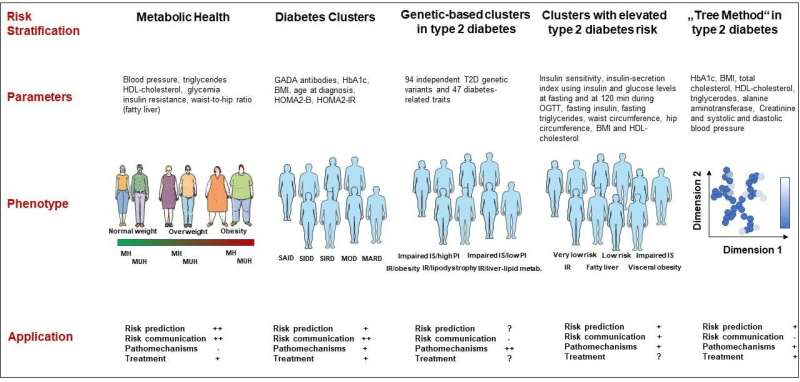
Norbert Stefan adds, “Do the novel cardiometabolic risk clusters also help to identify subgroups of people with distinct risk of cardiometabolic diseases?” To answer this question the authors of the present Review article discuss the findings from the most important data dimensionality reduction approaches that can be summarized under the term ‘cluster analysis’.
These studies were mostly done in patients with diabetes or in people at risk for type 2 diabetes. The cluster approaches are also based on routinely available, clinical variables, but can include more complex data, such as genetics. Among the subgroups deriving from these cluster analyses are people predominantly having low insulin secretion, insulin resistance, fatty liver, visceral obesity, mild age-related diabetes, mild obesity-related diabetes or other, more complex, phenotypes.
Norbert Stefan and Matthias Schulze conclude “Regarding cardiometabolic risk stratification, both the concept of metabolic health and the cluster approaches are not considered superior to established risk prediction models. However, both approaches might be informative to better predict cardiometabolic risk in subgroups, such as individuals in different BMI categories or people with type 2 diabetes.”
They also highlight that the applicability of the concepts by the treating physicians and communication of cardiometabolic risk with patients may be easier for the concept of metabolic health. The authors then point out that being metabolically healthy or unhealthy, or assigned to a specific cardiometabolic risk cluster, will in most cases be a transient allocation.
Furthermore, they conclude that the approaches to identify cardiometabolic risk clusters have provided evidence that they could be used to allocate individuals to specific pathophysiological risk groups. To what extent this allocation could improve risk assessment and treatment response still needs to be carefully studied.
More information:
Norbert Stefan et al, Metabolic health and cardiometabolic risk clusters: implications for prediction, prevention, and treatment, The Lancet Diabetes & Endocrinology (2023). DOI: 10.1016/S2213-8587(23)00086-4
Journal information:
The Lancet Diabetes & Endocrinology
Source: Read Full Article