
Leukemia relapse is still a major problem that impedes the success of hematopoietic cell transplant (HCT). Understanding the influence of treatment relevant variables in patients with refractory/relapsed acute leukemia (RRAL) is critical in the therapeutic decision making process. The population-based (the largest for haplo-identical group) real-world data suggest that RRAL patients who manage to receive a “total program” with prophylactic/preemptive donor lymphocyte infusion (p/pDLI) and intensified conditioning can tolerate and have good chances for survival.
Patients with acute leukemia who become refractory to initial or re-induction chemotherapy (refractory/relapsed acute leukemia [RRAL]) have poor prognosis, with limited therapeutic options with hematopoietic cell transplant (HCT) being the only opportunity to cure. Current strategies to decrease post-transplant relapse for patients with RRAL include more effective pre-transplant conditioning, safer donor lymphocyte infusion (DLI), and improved donor selection (including haplo-identical donor), though relevant real world data is scarce.
In the two largest series coming from international registries, most patients underwent HCT from matched sibling donors (MSDs) or unrelated donors (URDs) while haplo-identical donors (HIDs) only account for less than 10 percent of the population. Furthermore, only the impact of donor source and clinical factors on transplant outcomes were evaluated while treatment-related factors such as conditioning intensity or DLI were not analyzed. It is imperative to understand the influence of treatment relevant variables in patients with active disease in the therapeutic decision making process.
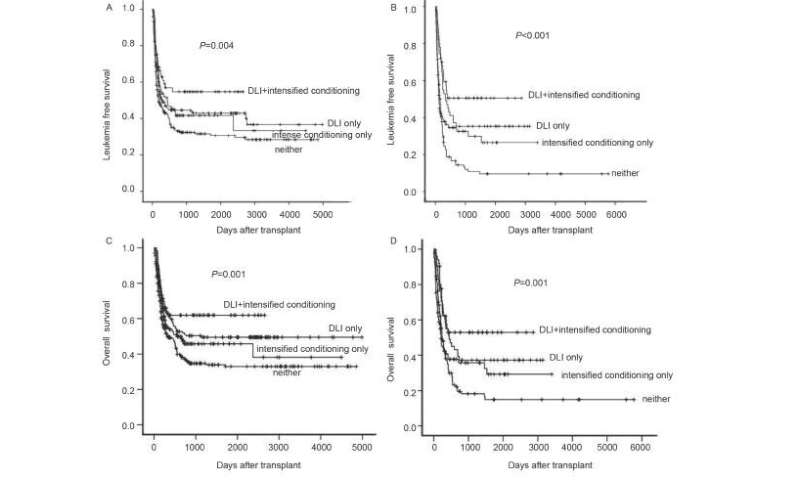
“To understand the influence of treatment relevant variables in patients with RRAL In practice, we analyzed the outcomes of 932 consecutive patients who underwent transplantation during relapse or primary induction failure to evaluate the impact of conditioning or DLI in RRAL,” said Professor Xiao-Jun Huang at Peking University Institute of Hematology, the corresponding author of this study. The results indicated that patients with RRAL can tolerate both interventions prophylactic/preemptive donor lymphocyte infusion (p/pDLI) and intensified myeloablative conditioning (intenseMAC) and achieve a really reasonable outcome. The 3-year leukemia free survival (LFS) rates were 56% for patients receiving both interventions and 30% for those with neither therapy by a landmark analysis.
“Furthermore, to evaluate whether conditioning, DLI, or the combined treatment have varying extents of impact among acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL) patients as well as among MSD and HID recipients, we performed multivariable analyses separately,” said Prof. Huang. p/pDLI was associated with significantly higher LFS than non-DLI for both AML and ALL patients without increasing nonrelapse mortality (NRM). IntenseMAC was linked to significantly lower relapse and higher LFS than nonintensified MAC despite higher NRM rates in ALL; there was no impact of intenseMAC in AML. Moreover, p/pDLI had superior outcomes in both MSD and HID transplant while intenseMAC only had influence on MSD outcomes. “So, RRAL patients receiving ‘total therapy’ by way of p/pDLI and intenseMAC have an improved chance for LFS, with p/pDLI being safer with a more extensive impact relative to intenseMAC,” said Prof. Huang.
Source: Read Full Article