The United States has a proven treatment to reduce HIV infection risk by up to 99%. The health system just needs to get better at offering it. In 2021, the country had over 36,000 new HIV diagnoses, yet PrEP (HIV pre-exposure prophylaxis) is used by fewer than one in four people who would benefit from it.
PrEP is preventive medicine—like statins to avoid heart disease—for HIV-negative people who risk infection through sex or drug use. Efforts to expand PrEP use include the U.S. Ending the HIV Epidemic (EHE) initiative to reduce new HIV infections by 90% by 2030. Health officials in Philadelphia, an EHE priority area, are partnering with LDI Fellows, the Penn Center for AIDS Research, and the Philadelphia Department of Public Health, in improving PrEP programs.
“Medical provider-, clinic-, and system-level barriers have made it hard to increase PrEP knowledge, access, and uptake in communities in Philadelphia that could benefit from it,” said Kathleen Brady, director and medical director of the Health Department’s Division of HIV Health. “The collaboration is helping us to identify these barriers and address them.”
Other PrEP studies from LDI Fellows focus on people marginalized because of race or ethnicity, LGBTQ+ status, age, or substance use disorder.
Normalizing PrEP, raising awareness
PrEP access is inequitable: People who are Black or Hispanic/Latino are over-represented in new HIV diagnoses and women are 19% of new diagnoses, yet 10% or fewer of individuals in these groups obtain PrEP prescriptions.
Why? Stigma. LDI Senior Fellow Sarita Sonalkar, MD, MPH, said that HIV and sex are often stigmatized in women. Devaluing people who use drugs, LDI Associate Fellow Maria Christina Herrera, MD, MSHP, said, “contributes to both the overdose epidemic and the HIV epidemic.”
Philadelphia collaborations by LDI Senior Fellow Stephen Bonett, Ph.D., RN, suggest approaches for destigmatization. One is universal PrEP counseling. “Everyone gets the info,” he said. “It’s just part of comprehensive sexual health services.”
Another is culturally relevant, humble care that acknowledges the cultural background many people bring to relationships and how little we know about others. “This puts patients and medical providers on an equal plane,” Bonett said. Having health workers with lived experience in the community also builds trust.
Herrera agrees: Trusted messengers reduce stigma. For people getting substance use care, certified recovery specialists—peers with lived experience and training in nonjudgmental communication—are “a surefire way to get patients to hear about PrEP.”
The messengers LDI Senior Fellow Dalmacio Flores, Ph.D., ACRN, works with are parents of LGBTQ+ children. Some communities have persistent stigma that particularly affects queer youth of color, he said.
Flores was part of a team that surveyed 400 self-identified Black gay and bisexual U.S. males, aged 18 to 29. Family support was associated with lower stigma and higher positivity about PrEP. However, open communication with parents about sex and drugs was linked to higher PrEP stigma, possibly because of parental discomfort and cultural attitudes about HIV. The findings were published in the journal Sexually Transmitted Diseases.
The findings show the need for Flores’ Parents ASSIST program of animated information videos, piloted over the past few years, with a randomized controlled effectiveness trial in the works. “Parents are with their young person everyday,” Flores said. “They often provide health insurance, so inclusive, nonstigmatizing conversations about HIV and PrEP and normalizing insurance for health care around sexual behavior is more powerful than any public health message.”
Presenting PrEP as preventive, “like the pill but for gay kids,” normalizes it, Flores said. Flores also helps community and religious organizations, schools, and nonprofit groups communicate with LGBTQ+ youth about sexual health.
Nonjudgmental presentation of PrEP promotes interest in the treatment. Associate LDI Fellow Caroline Darlington, MSN, with LDI Senior Fellow Peggy Compton, Ph.D., RN, surveyed 233 women vulnerable to HIV infection about PrEP awareness before seeing an informational video, and their intention after the video to start PrEP within three months. Overall, 42% were aware of PrEP before, but after learning about PrEP, 63% intended to initiate.
The study was part of the Just4Us trial led by LDI Senior Fellow Anne Teitelman, Ph.D., who said these results show that “awareness and knowledge are key. PrEP has been approved for 12 years, but women who haven’t heard of it are hesitant, like we saw with the COVID vaccine.” Many cisgendered women who know of PrEP think it is for gay men, Teitelman said, so publicizing that PrEP is established HIV prevention for anyone—cis, trans, gay, straight, using or not using drugs—could increase uptake.
Women who reported use of prescription opioids or multiple drugs had particularly high intentions to start PrEP after hearing about it. To Darlington, who treats women with substance use disorders, this suggests opportunities for PrEP education during drug treatment.
Integrating PrEP into health care
With LDI Senior Fellows Sarah Wood, MD, MSHP, and Nadia Dowshen, MD, MSHP, Herrera interviewed providers about their records of prescribing PrEP or medication for opioid use disorder to people aged 16 to 29. They showed that training prescribers to be comfortable offering PrEP might correct low use in this group. Herrera plans to create a decision aid, using patient and provider input, to guide nonstigmatizing patient-provider conversations about PrEP.
To integrate PrEP with family planning services, Sonalkar, with LDI Senior Fellow Shimrit Keddem, Ph.D., MPH, asked people visiting a family planning clinic how they felt about including HIV screening and PrEP discussions in their visit for abortion, early pregnancy loss, or contraception.
Overall, this was “very acceptable,” Sonalkar said, although for early pregnancy loss, many preferred the discussion at a later visit. Particularly helpful was information about women’s HIV risks and PrEP effectiveness at lowering them. “Patients felt that the screening just opened the door to a real conversation,” Sonalkar said. “They wanted frank, but private, nonjudgmental discussions about PrEP.”
The study called for provider training through public health departments to raise confidence about PrEP conversations. The U.S. Preventive Services Task Force now recommends PrEP for people at risk of HIV infection. Sonalkar said more statements and guidelines from influential societies such as the American College of Obstetricians and Gynecologists would show that HIV screening and PrEP are essential sexual health services.
Sonalkar practices universal PrEP counseling, saying, “I tell all patients about PrEP, even if they don’t seem to have risks. Awareness is low, so just telling someone increases knowledge about it.”
Removing barriers to PrEP
Using PrEP requires multiple steps: a negative HIV test, a prescription, and quarterly blood-test monitoring. Bonett evaluated Philadelphia’s effort to remove PrEP barriers via low-threshold, “one-stop-shop” care from community clinics. This means “no hoops to jump through, so it’s super easy to come in,” Bonett said. He found the strategy connected people to housing, food, and jobs.
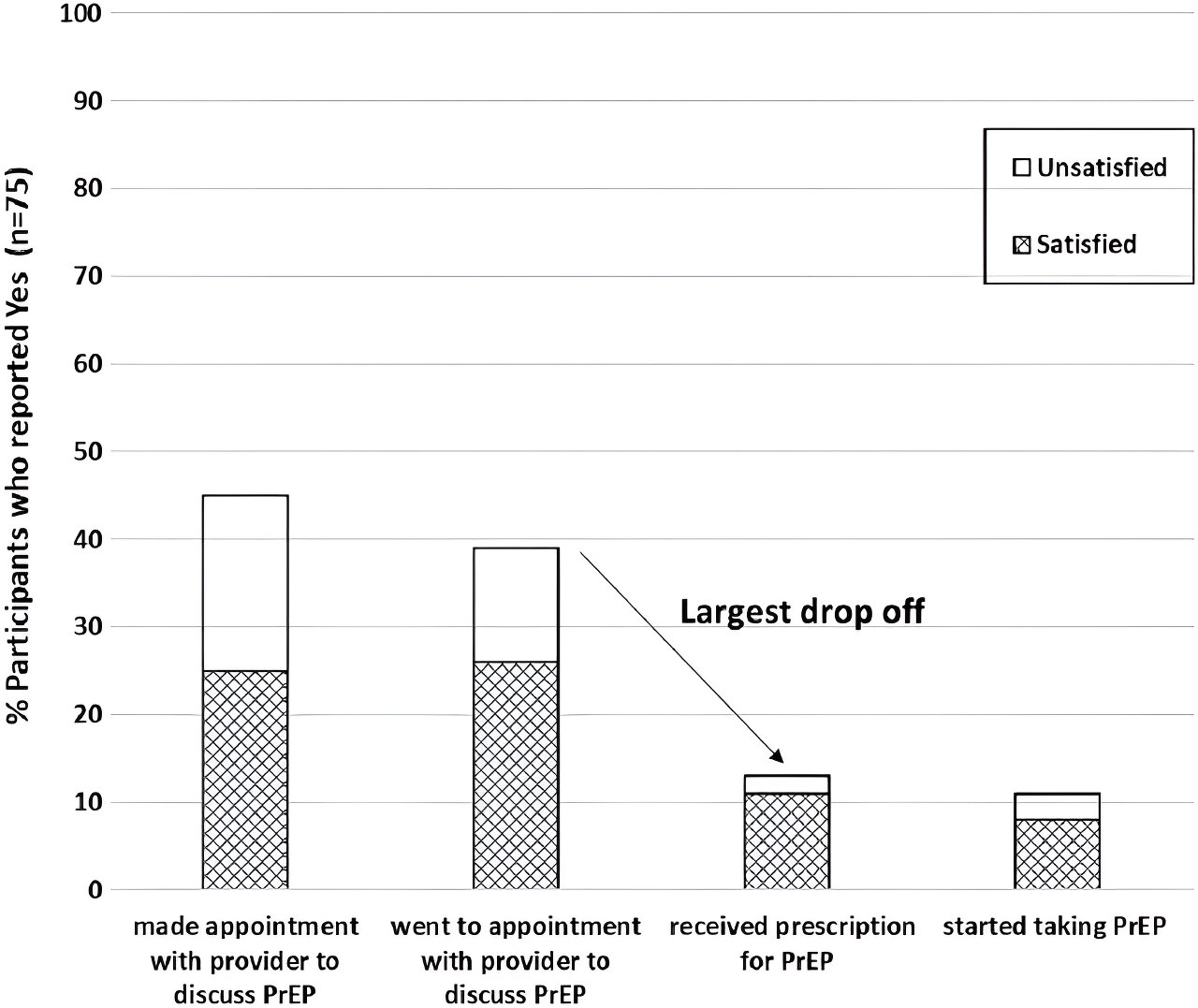
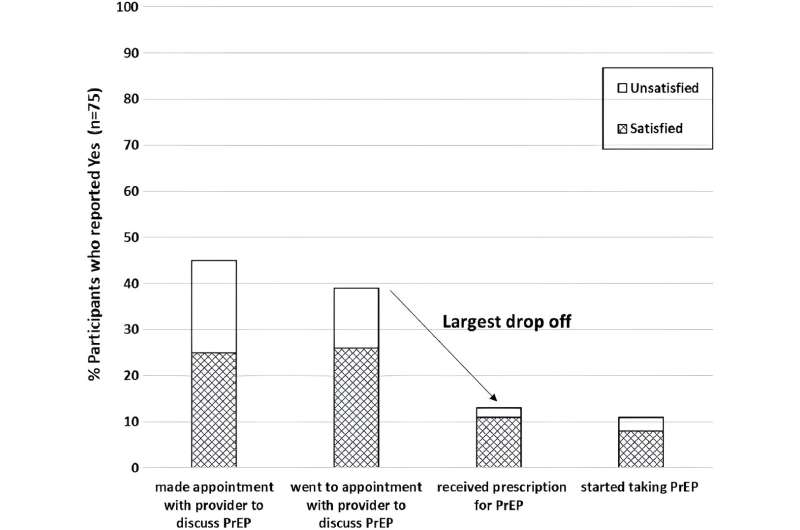
When patients and providers must cover multiple issues in one visit, competing needs can be a barrier to integrating care. “It takes a while to go over PrEP with someone,” Teitelman said. Her Just4Us randomized controlled trial in New York City and Philadelphia tested a counseling-and-navigation intervention that could help busy providers integrate PrEP into care and increase uptake in cisgender women. The results were published in AIDS and Behavior.
Just4Us participants had “few resources and many challenges,” Teitelman said, such as poverty, homelessness, substance use, and incarceration. They were enthusiastic about the intervention, but many faced ongoing barriers such as a lack of transportation and childcare for PrEP’s multiple appointments. Most people enrolled in Just4Us had insurance thanks to Obamacare, Teitelman said, but recommended blood-test monitoring might have copays.
Innovations to Make PrEP More Equitable
A potential solution is TelePrEP, a new Philadelphia program for providing PrEP online that Bonett is studying. From a website, individuals can schedule a telehealth appointment about PrEP, and get a mailed kit for self-collecting a sample for the required HIV test. If appropriate, PrEP prescribing and provision is online and through the mail.
Researchers and PrEP providers are interested in next-generation HIV prevention products including longer-acting implants, vaginal rings, and injections. “The latest formulations have immense potential for people for whom daily medication doesn’t make sense,” said Herrera. “We heard a lot of interest from providers.”
Multipurpose products are also intriguing. Sonalkar said family planning provides lessons about integrating new technology into preventive care, such as birth control pills that contain iron supplements. She envisions options that combine PrEP with contraception by pill, injection, or implant. New products tend to be expensive, she said, so ensuring insurance coverage is vital.
LDI Senior Fellow José Bauermeister studies these new products and said they could reshape the HIV prevention and treatment landscape. He advises, however, that they have similar issues as current PrEP formulations around cost, delivery, uptake, and persistent use, particularly in resource-constrained settings and marginalized groups. He calls for robust multisector research to increase PrEP options for effective, equitable use.
Priorities raised by LDI Fellows—fair access to new products, insurance coverage for PrEP, and integrated treatment that’s accessible and culturally humble—are federal and city goals, Brady said. The next few years will include working with Penn and community partners to “create an HIV prevention system that meets people where they are at and gives them the tools that they need to protect themselves and their communities.”
More information:
Anne M. Teitelman et al, A Randomized Controlled Pilot Study of Just4Us, a Counseling and Navigation Intervention to Promote Oral HIV Prophylaxis Uptake Among PrEP-Eligible Cisgender Women, AIDS and Behavior (2023). DOI: 10.1007/s10461-023-04017-z
Donte T. Boyd et al, The Role of Family Support and Communication on PrEP Attitudes and Stigma Among Black Men who have Sex with Men (BMSM), Sexually Transmitted Diseases (2023). DOI: 10.1097/OLQ.0000000000001832
Journal information:
AIDS and Behavior
,
Sexually Transmitted Diseases
Source: Read Full Article