 Reviewed
Reviewedtakethehealth.com
 Reviewed
ReviewedMen who are overweight or obese at age 18 have a higher risk of 17 different cancers later in life. This has been shown in a study at the University of Gothenburg. The research also describes how the youth obesity epidemic is expected to affect the cancer situation over the next 30 years.
In August, a study on higher cancer risk in men who had lower aerobic fitness recorded at the time of compulsory conscription for military service at the age of 18 was presented. The results were independent of any overweight or obesity at conscription.
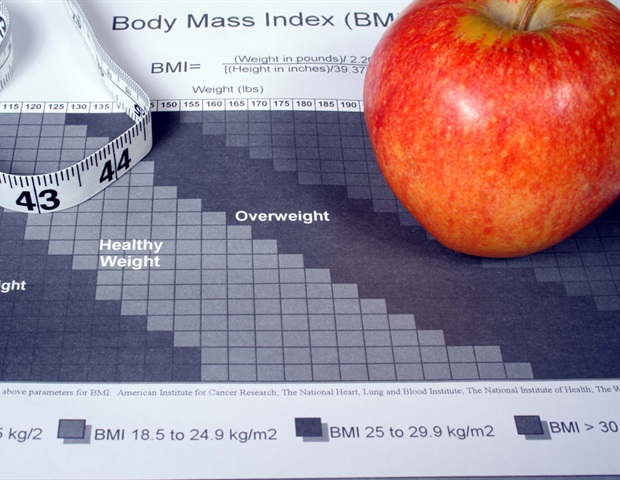
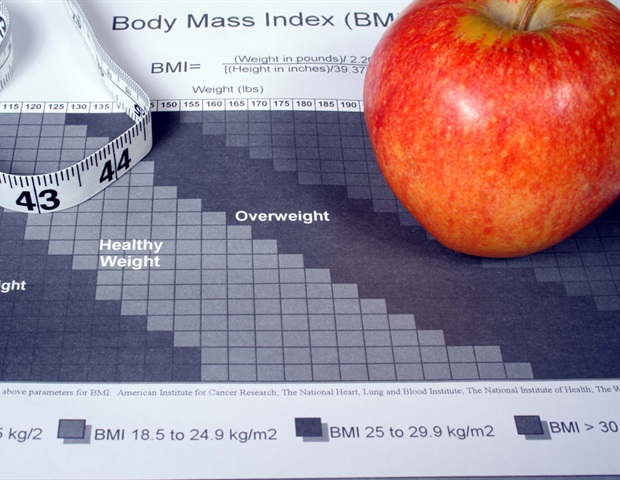
In two new studies published in the journals Obesity and Cancer Medicine, the same research team is now focusing on body mass index (BMI), while the results are independent of the participants' aerobic fitness level. And it turns out that higher BMI at age 18 can be linked to even more cancers later in life than poor fitness at the same age.
High BMI at conscription was associated with a higher risk of 17 cancers: lung, head and neck, brain, thyroid, esophageal, stomach, pancreatic, liver, colon, rectal, kidney, and bladder cancer, as well as malignant melanoma, leukemia, myeloma, and lymphoma (both Hodgkin's and non-Hodgkin's).
For several of the cancer types, the risk was elevated already at a BMI of 20-22.4, within the usually used range of normal weight (18.5-24.9). These included cancers of the head and neck, esophagus, stomach, pancreas, liver, and kidney, as well as malignant melanoma and non-Hodgkin's lymphoma.
This suggests that the current definition of normal weight may be applicable primarily for older adults, while an optimal weight as a young adult is likely to be in a lower range. Our research group has drawn similar conclusions regarding BMI in early adulthood and later cardiovascular disease."
Maria Åberg, professor of family medicine at Sahlgrenska Academy at the University of Gothenburg and senior author
One cancer type studied deviated from the pattern; prostate cancer was more common among those who were not overweight or obese at the time of enlistment. One likely explanation is that men of normal weight are more likely to seek care for prostate problems, leading to more early healthcare contacts and diagnoses.
The link with high BMI was strongest for abdominal cancers, including cancer of the esophagus, stomach, and kidney, with a three to four times higher risk for obese men at enrolment. An unhealthy weight seemed to explain about 15-25% of cases of these cancers in Sweden today.
In 30 years, the researchers expect an increase in the proportion of cancer cases linked to youth overweight and obesity, calculated based on overweight and obesity in today's 18-year-old men in Sweden. For cancer of the stomach, the proportion rises to 32% and for cancer of the esophagus to 37%. Based on the current prevalence of youth overweight and obesity in the United States, more than one in two cases of these two cancers could be linked to high BMI in the late teenage years in 30 years.
Aron Onerup is a postdoc at Sahlgrenska Academy at the University of Gothenburg, and St. Jude Children's Research Hospital in Memphis, USA, and first author of the studies.
"Overweight and obesity at a young age seems to increase the risk of developing cancer, and we see links between unhealthy weight and cancer in almost every organ. Given the alarming trend of obesity in childhood and adolescence, this study reinforces the need to deploy strong resources to reverse this trend," he says.
The researchers also studied mortality rates after cancer diagnosis in this group. Of the 1,489,115 men studied who enlisted in Sweden between 1968 and 2005, 84,621 were diagnosed with some form of cancer during the follow-up period.
The analyses showed that men who were overweight or obese were 2-3 times more likely to die within five years of being diagnosed with skin cancer, Hodgkin's lymphoma and thyroid, bladder, and prostate cancer, and 1.4-2 times more likely to die from cancers of the head and neck, rectum, and kidneys.
University of Gothenburg
Onerup, A., et al. (2023). Cardiorespiratory fitness and BMI measured in youth and 5‐year mortality after site‐specific cancer diagnoses in men—A population‐based cohort study with register linkage. Cancer Medicine. doi.org/10.1002/cam4.6553.
Onerup, A., et al. (2023). Associations between BMI in youth and site-specific cancer in men—A cohort study with register linkage. Obesity. doi.org/10.1002/oby.23942.
Posted in: Medical Research News | Medical Condition News
Tags: Bladder, Bladder Cancer, Body Mass Index, Brain, Cancer, Cancer Diagnosis, Cardiovascular Disease, Children, Colon, Healthcare, Hodgkin's Lymphoma, Hospital, Kidney, Leukemia, Liver, Lymphoma, Malignant, Medicine, Melanoma, Mortality, Myeloma, Neck, Non-Hodgkin's Lymphoma, Obesity, Pancreas, Prostate, Prostate Cancer, Research, Skin, Skin Cancer, Stomach, Thyroid