National guidelines are needed for health professionals to navigate discussions about past traumas with pregnant women, according to new research published today.
The research, carried out by a team from the School of Community Health and Midwifery at the University of Central Lancashire (UCLan), is published in PLOS ONE.
The study found that that while most women agreed that trauma discussions can be valuable, if not approached sensitively they can be intrusive and trigger painful memories. The findings also raised concerns about the support available for maternity care professionals who may not feel equipped to explore challenging topics such as domestic or sexual abuse, childhood trauma and birth trauma without adequate guidelines or referral pathways, and may themselves find some of the questions triggering.
Joanne Cull, a midwife and Ph.D. student at UCLan, led the project.
She said, “One in three pregnant women in the UK (250,000 each year) have suffered trauma, such as abuse or violence, in childhood or adulthood. Because awareness of the long-term effects of trauma on health and well-being has grown, there has been a move toward asking pregnant women about previous trauma, usually at the first appointment. No national guidance on this has been published in the UK so NHS Trusts have implemented this on a piecemeal approach.”
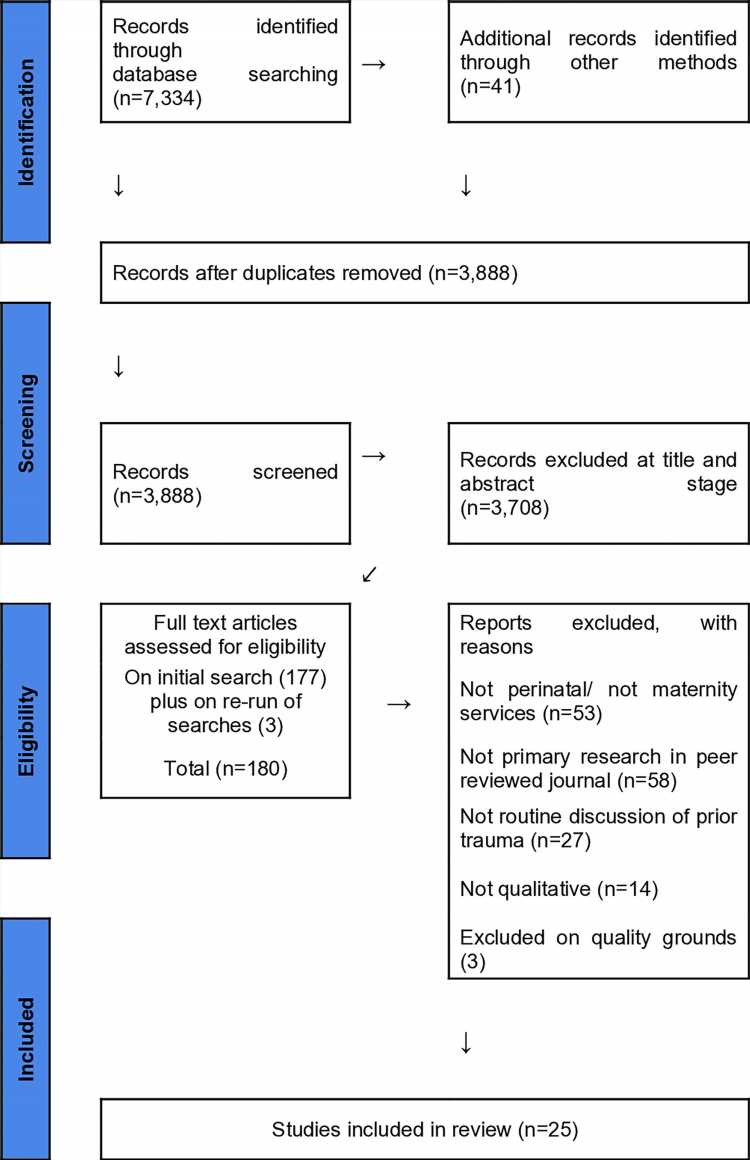
The PLOS ONE paper, “Views from women and maternity care professionals on routine discussion of previous trauma in the perinatal period: A qualitative evidence synthesis,” is a systematic review of all the published research in this area. It includes UK data and studies in comparable high-income countries, mainly Australia and the U.S., which were published between 2001 and 2022. The review brings together 25 research papers which cumulatively included the views and experiences of 1,602 women and 286 health care professionals.
The review is part of a larger study that was designed with the input of women who have suffered trauma or abuse themselves, experts from charities including The Survivors Trust and the Birth Trauma Association, and maternity care professionals. Joanne and the team are using findings from the review and from subsequent interviews to develop guidelines for routine discussion of previous trauma in the perinatal period.
“Our review suggests specific areas of training that are necessary for maternity care professionals to feel confident in supporting women to share their trauma histories,” said Joanne.
“The focus of trauma discussions should not be on obtaining specific details of past trauma, but rather exploring what resources, support, and adjustments to their care would be helpful. There is no point asking such sensitive questions if you don’t know where to signpost parents for support and this is where national guidelines would be useful.”
“In addition, it is important that women are forewarned of the discussion, including any limits to confidentiality, and that disclosure of past trauma is entirely voluntary. Providing continuity of care, where women can build a trusting relationship with their midwife, can also be helpful. It is crucial that all women are given access to support and resources so they can seek help independently if they choose not to disclose their histories.”
Mom-of-one Toyin Adeyinka has previous trauma that resulted in significant mental health problems after birth. She has worked with the team on the study. She said, “Joanne’s research has shown how important it is to listen to people who have experienced trauma, in particular childhood trauma. The lasting impact of trauma isn’t talked about enough.”
“Discussing trauma has to be done safely. Staff need to be trained on how to support a person after they have disclosed trauma, and receive support themselves. Discussing trauma can be very empowering, especially when talking about sexual abuse. There is so much shame and judgment, acknowledging it safely changes the narrative and encourages more people to share.”
Kim Thomas, CEO of the Birth Trauma Association, said, “Many of the women who approach the Birth Trauma Association are fearful of giving birth, either because their previous experience of birth was traumatic, or because they have been through some other form of trauma, such as sexual abuse.”
“We know that previous trauma makes women vulnerable—research shows that survivors of sexual abuse, for example, are 12 times more likely to experience birth as a traumatic event. Women in this situation need to be supported sensitively so that their experience of birth is a positive one, not one that leaves them re-traumatized.”
“We believe that Joanne Cull’s research into trauma-informed care is immensely valuable in identifying how caregivers can be trained to help women to disclose trauma, to respond with sensitivity and to support women in a way that minimizes the risk of them experiencing birth as traumatic.”
The research also found that women with limited English face additional barriers because they may not feel comfortable disclosing past abuse in the presence of an interpreter, or a partner or family member who is interpreting.
In addition, findings suggest that many pregnant women are unaware of the extent of the trauma they have suffered, or its impact on their lives. This highlights the difficulty of discussing trauma with women who will be at very different stages of recovery.
Joanne added, “Women often feel especially vulnerable during pregnancy and so discussions at this time can be even more difficult. National guidelines and specific training for staff on this issue would benefit not only parents, but also clinicians, who can find trauma discussions challenging.”
More information:
Joanne Cull et al, Views from women and maternity care professionals on routine discussion of previous trauma in the perinatal period: A qualitative evidence synthesis, PLOS ONE (2023). DOI: 10.1371/journal.pone.0284119
Journal information:
PLoS ONE
Source: Read Full Article