The COVID-19 pandemic had a substantial and diverse impact on cancer care, but we still don’t know how this affected prognosis, according to a study published today in eLife.
The findings suggest that more and better-quality research is needed to understand the full impact of COVID-19 on people with cancer, specifically in low-income settings and looking at longer-term outcomes.
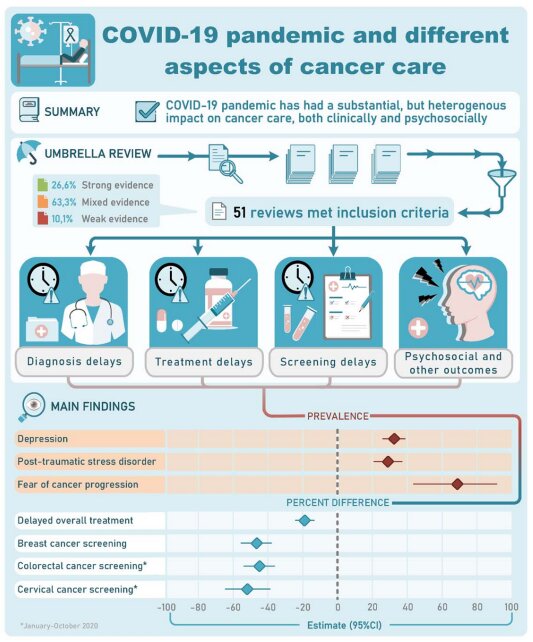
The authors conducted an umbrella review of systematic reviews, which collect and summarize all studies and evidence on a well-defined topic. Systematic reviews are commonly used as evidence to guide public health and policy decision-making, but their quality and impact depends on the methods used and the quality of the individual studies the reviews include.
“Several systematic reviews have examined the impact of COVID-19 on cancer care, but they evaluated different outcomes and periods of the pandemic, and so the findings are rather fragmented and the rigor of the methods used is unclear,” explains lead author Taulant Muka, a medical epidemiologist at the Institute of Social and Preventive Medicine, University of Bern, Switzerland. “Well-designed studies for a comprehensive and rigorous assessment of the impact of COVID-19 on several aspects of cancer are essential to understand gaps and learn lessons for future pandemics.”
To address this, the team performed an umbrella review to assess the amount and geographical breadth of the available evidence. Then they summarized the impact of COVID-19 on screening, diagnosis and treatment of cancer, as well as financial, psychological and social aspects of living with the disease.
They searched the scientific literature and identified 51 articles that met their criteria, with most providing data from different countries and only two focusing on a single country. When they evaluated both the methodological rigor of each review, and the individual studies they included, only two reviews scored as moderate to high-quality, and the rest for low or critically low quality.
The authors then summarized the main evidence on aspects of cancer care including changes to treatment regimens, delays or cancelations to screening or treatment, numbers of diagnoses, financial distress, social isolation and uptake of telemedicine.
Different degrees of delays and cancelations were reported, with low and middle income countries and countries that implemented lockdowns experiencing more delays and cancelations.
There was a significant upwards shift in the use of telemedicine, but little available evidence on how patients found its use, or the challenges, benefits and costs of its implementation.
A consistent theme was a deterioration in psychosocial well-being in cancer patients, such as increased depression and anxiety levels and feelings of social isolation; however, most reviews did not compare this with pre-pandemic data.
Finally, although several guidelines were produced in the midst of the pandemic to support clinicians caring for people with cancer, most recommendations were based on expert opinion rather than quantitative evidence. For example, a comparison of recommendations for radiotherapy timing and dose before and after the pandemic, showed a shift from established higher-quality evidence used before the pandemic to recommendations based on lower-quality evidence and expert opinion during the pandemic.
“The main take-home message provided by the 51 reviews we looked at is that there have been modifications, delays and cancelation of screening, diagnosis and treatment, and patients with cancer may have experienced additional psychological, social and financial distress,” says senior author John P.A. Ioannidis, Professor of Epidemiology and Population Health at Stanford University, U.S.
“Nevertheless, the appraisal is based on limited and low-quality evidence and data derived from high-income countries, with little understanding of the consequences of COVID-19 on cancer care in low- or middle-income settings, or on any adverse impact of COVID-19 on cancer prognosis and survival.”
More information:
Taulant Muka et al, An umbrella review of systematic reviews on the impact of the COVID-19 pandemic on cancer prevention and management, and patient needs, eLife (2023). DOI: 10.7554/eLife.85679
Journal information:
eLife
Source: Read Full Article