
By quantifying the probability of infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in accordance with its viral load after a high-risk contact, researchers from France, Spain, and the United Kingdom show a substantial correlation of transmission probability and viral load increase in variants of concern. Their paper is published in the prestigious journal eLife.
Even though aerosols and respiratory droplets have been demonstrated quite early as principal routes of transmission of SARS-CoV-2 – a causative agent of the ongoing coronavirus disease (COVID-19) – viral load as a driver of infectiousness has been established, but thus far not quantified.
In light of the fact that high-risk contacts are developed before the index case has been diagnosed, it's no wonder that we lack information on viral load levels at contact time. Moreover, since SARS-CoV-2 variants of concern are associated with larger viral loads, its exact contribution becomes a primary question of interest.
Moreover, as vaccines and antivirals have the potential to substantially reduce the amount of viral shedding, it is pivotal to understand how they may actually contribute to reducing viral transmission. All of this means that we need to take a deep dive into the available data to make any reliable conclusions.
In this new study, led by Dr. Aurélien Marc from the University of Paris in France, the impact of viral load on infectiousness was quantified with the use of a large amount of data obtained in prospective cohorts of index and contact cases.
Statistical models for viral transmission
For the purposes of this study, this research group used data from a clinical trial on hydroxychloroquine efficacy that was conducted in Spain between March 17 and April 28, 2020. In addition, detailed statistical modeling has been pursued.
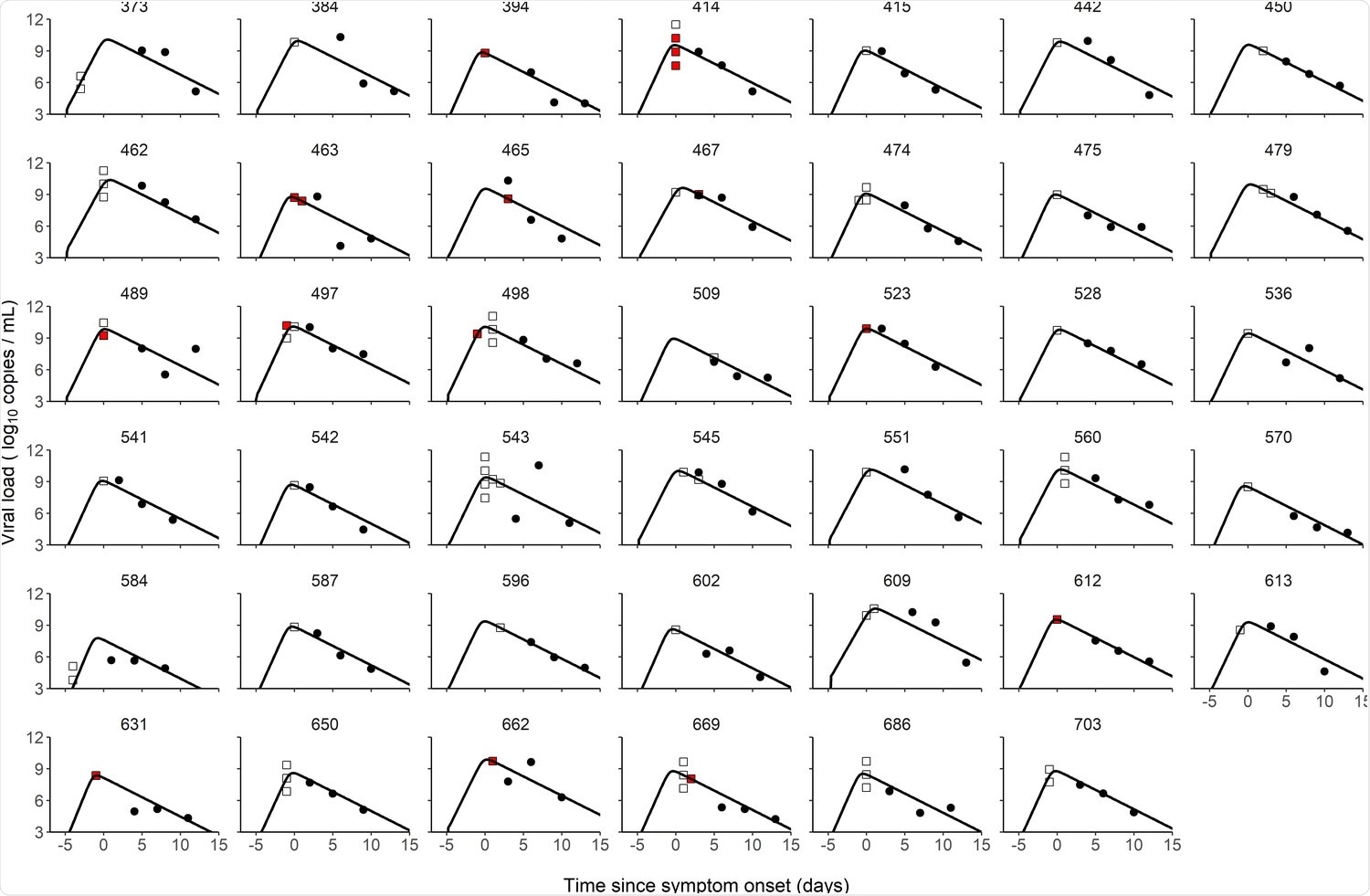
The role of viral load on the probability of spread was studied in detail by reanalyzing many different data points with the use of a within-host model of viral dynamics. In short, the researchers have reconstructed viral load levels of the index cases at the time of high-risk contact in order to infer its relationship with the probability of SARS-CoV-2 transmission.
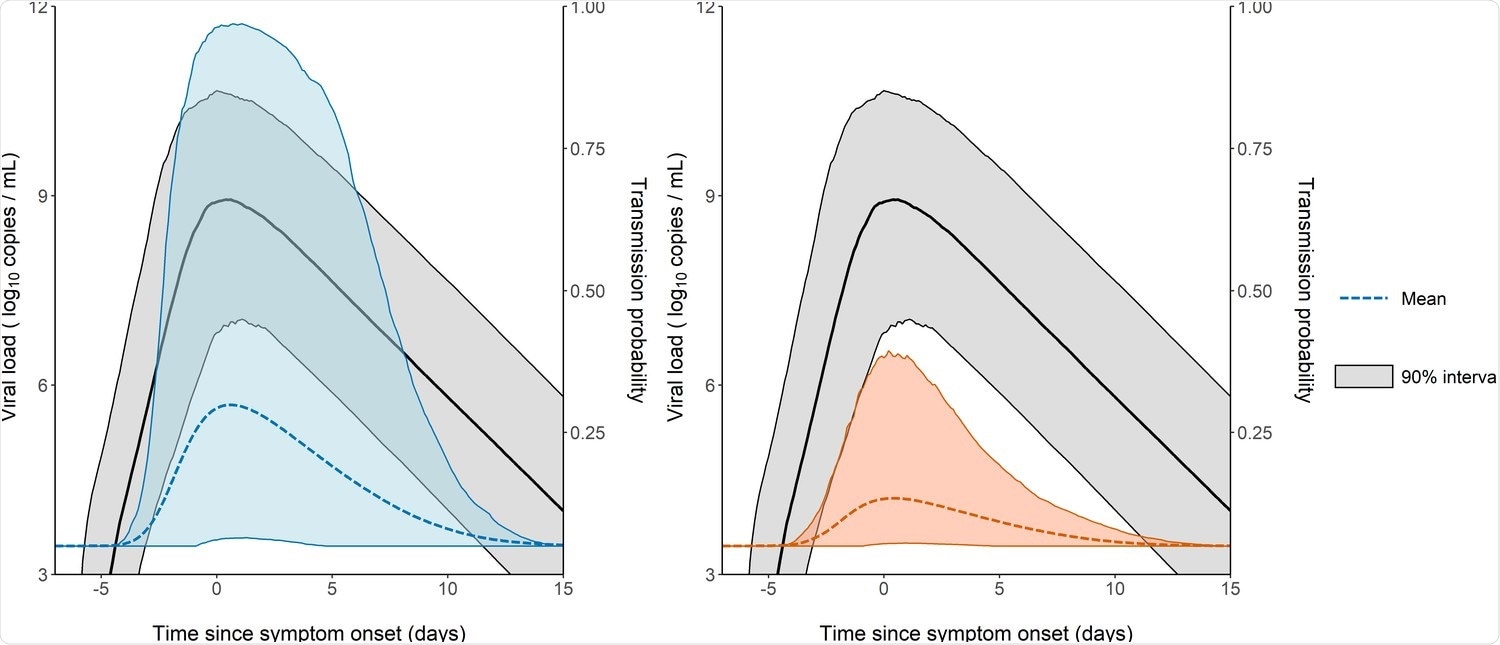
Furthermore, they have utilized the model to predict how changes in viral load levels actually impact the probability of transmission – both in instances when confronted with a variant of concern or when an individual has been given a vaccine to confer at least a partial protection against viral replication.
Viral loads and subsequent spread of SARS-CoV-2
The study has shown that the effect of viral load was much more significant in household contacts than in non-household contacts, with specific transmission probability that increased to as much as 48% when the viral load exceeded 1010 copies per milliliter. Furthermore, the transmission probability peaked at symptom onset, although there were significant individual variations.
As we already know that the viral load is increased by 2-8 times with variants of concern, and if we assume no changes in the pattern of contacts across these variants, the model in this study predicts that larger viral load levels could increase transmission probability from 24% to 58% in household contacts, as well as from 15% to 39% in non-household contacts.
Of course, reporting high-risk contacts can be prone to several biases, and household contacts may not be unique and could occur multiple times, which is something that will have to be addressed by studies in the future (as well as the use of face masks, which was not taken into account here).
Predicting infection patterns
In conclusion, this study quantifies the probability of infection in accordance with viral load level following a high-risk contact. This relationship is predictive of changes in virus paradigm, which is a result of emerging novel variants, as well as the rollout of vaccination.
"Vaccination rollout is expected to confer a large level of protection, partly due to lower virus carriage in infected individuals," said study authors in this eLife paper. "However, the exact magnitude of this decrease is difficult to quantify and depends on the design of the study that relied on systematic testing or included only symptomatic individuals," they add.
In any case, these findings may be of interest to infectious disease modelers and policymakers. Still, there is uncertainty on the predictions of individual trajectories, which is inherent to the nature of SARS-CoV-2; therefore, additional modeling studies on the topic will be needed to increase the prognostic potential of these types of approaches.
- Marc, A. et al. (2021). Quantifying the relationship between SARS-CoV-2 viral load and infectiousness. eLife. 10.7554/eLife.69302, https://elifesciences.org/articles/69302
Posted in: Medical Research News | Disease/Infection News
Tags: Clinical Trial, Coronavirus, Coronavirus Disease COVID-19, Efficacy, Hydroxychloroquine, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Vaccine, Virus

Written by
Dr. Tomislav Meštrović
Dr. Tomislav Meštrović is a medical doctor (MD) with a Ph.D. in biomedical and health sciences, specialist in the field of clinical microbiology, and an Assistant Professor at Croatia's youngest university – University North. In addition to his interest in clinical, research and lecturing activities, his immense passion for medical writing and scientific communication goes back to his student days. He enjoys contributing back to the community. In his spare time, Tomislav is a movie buff and an avid traveler.
Source: Read Full Article